ESE Bite-size Bulletin
7 October 2022
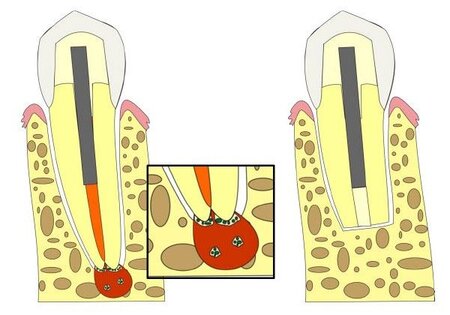
Apical periodontitis is an inflammatory reaction in the periapical tissues caused by microorganisms of endodontic origin and their by-products. Primary apical periodontitis is treated by root canal treatment, performed under strict infection control, using antiseptic measures, followed by root canal filling and closure of the tooth with a sealing restoration. In some cases the primary treatment is unsuccessful and the disease may persist. The causes of an unsuccessful treatment may include untreated root canal anatomy, insufficient irrigation, inadequate instrumentation, incomplete filling of the root canal system, or a combination of these. However, even if all the procedural steps are followed, intra-radicular microorganisms may still persist and survive in inaccessible ramifications and anastomoses of the main and accessory canals, and within the dentinal tubules.
Failure of primary root canal treatment may be addressed via a non-surgical (conventional retreatment) or a surgical approach (apical surgery), as well as by tooth extraction.
The aim of this systematic review was to assess if surgical retreatment was more effective for treating persistent apical periodontitis following initial root canal treatment compared with conventional root canal retreatment (Bucchi et al., 2022).
The review only included studies in which both treatment modalities were included (Bucchi et al., 2022). After the electronic search and study screening, five studies were included, including four clinical trials (Danin et al., 1996; Riis et al., 2018; Estrela et al., 2014; Prati et al., 2018) and one observational study (Liu et al., 2021).
Studies were heterogeneous with an overall high or moderate risk of bias. The main flaws included; the randomization process was not described, blinding of patients and personal data was not possible, and/or the baseline characteristics of the patients in both groups were different, among others.
The findings indicated that apical surgery resulted in better results regarding periapical healing (82.9% versus 71.7%) and a reduced need for further intervention (7.1% versus 18.31%). Regarding tooth survival, a higher survival rate was detected in the non-surgical treatment group (88.19% versus 84.04%). However, it should be noted that the inclusion criteria for the surgical and non-surgical groups differed, as the non-surgical group included teeth with both primary and secondary apical periodontitis, whereas only teeth with secondary infection were included in the apical surgery group.
Notably, several of the critical outcomes intended to be analyzed in the systematic review, such as pain, tenderness, swelling, need for medication, presence of sinus tract, satisfactory soft-tissue healing and tooth mobility were not reported by any of the included studies. Future clinical trials comparing both procedures should measure these outcomes.
As a result, all the review findings should be taken with caution, as they are mostly based on studies with a high risk of bias.
The information from this review will together with clinical expertise and patient preferences form the basis for development of S3-level clinical practice guidelines and associated recommendations
Controlled clinical trials comparing the clinical and patient-related outcomes of apical surgery and conventional endodontic treatment are still needed and should be conducted and reported according to consolidated standards like the CONSORT statement (Moher et al., 2010).
References
Bucchi, C., Rosen, E. & Taschieri, S. (2022) Non-surgical root canal treatment and retreatment versus apical surgery in treating apical periodontitis: A systematic review. International Endodontic Journal, doi: 10.1111/iej.13793.
Moher. D., Hopewell, S., Schulz, KF., Montori, V., Gøtzsche, PC., Devereaux, PJ. et al. (2010) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. British Medical Journal, 10(1), 28-55.
Danin, J., Strömberg, T., Forsgren, H., Linder, L.E. & Ramsköld, L.O. (1996) Clinical management of nonhealing periradicular pathosis. Surgery versus endodontic retreatment. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 82, 213– 217.
Estrela, C., Silva, J.A., Decurcio, D.A., Alencar, A.H.G., Estrela, C.R.A., Faitaroni, L.A. et al. (2014) Monitoring nonsurgical and surgical root canal treatment of teeth with primary and secondary infections. Brazilian Dental Journal, 25, 494– 501.
Liu, S.Q., Chen, X., Wang, X.X., Liu, W., Zhou, X. & Wang, X. (2021) Outcomes and prognostic factors of apical periodontitis by root canal treatment and endodontic microsurgery-a retrospective cohort study. Annals of Palliative Medicine, 10, 5027– 5045.
Prati, C., Azizi, A., Pirani, C., Zamparini, F., Iacono, F., Montebugnoli, L. et al. (2018) Apical surgery vs apical surgery with simultaneous orthograde retreatment: a prospective cohort clinical study of teeth affected by persistent periapical lesion. Giornale Italiano di Endodonzia, 32, 2– 8.
Riis, A., Taschieri, S., Del Fabbro, M. & Kvist, T. (2018) Tooth survival after surgical or nonsurgical endodontic retreatment: long-term follow-up of a randomised clinical trial. Journal of Endodontics, 44, 1480– 1486.
